Cervical Laminectomy +/- Fusion
Cervical stenosis can place pressure on and compress the spinal cord. If most of the compression is in the back, the cervical stenosis can be treated with a posterior cervical laminectomy. The objective of this procedure is to remove the lamina (and spinous process) to give the spinal cord more room.
The prime aim of this procedure is to prevent progression of the spinal cord damage (myelopathy) and arrest further loss of function. If this is achieved without any loss of function, then the procedure is regarded as successful. The positive neurological results of the laminectomy are variable, since some people have more extensive disease than others. In general, after the laminectomy most patients can expect to regain some spinal cord function in the form of :
- Improvement in their hand function and walking capabilities
- Less or no numbness in their hands (if there was a lot of numbness prior to the surgery, it probably won’t go away completely)
Cervical Laminectomy Risks and Complications:
As with all other cervical surgical procedures, the principal risk is deterioration in neurological functioning after the surgical procedure. Other risks include :
- Infection
- Bleeding
- Deep vein thrombosis, pulmonary embolism
- Ongoing pain
- Late instability
- Re-operation
- No improvement
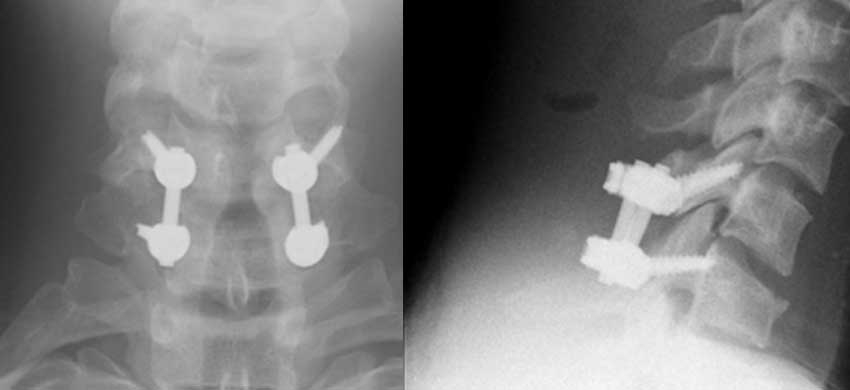
Cervical fusion:
The procedure is sometimes performed with a cervical fusion at the same time. This is done electively if instability is detected in the pre-operative evaluation or, if at the time of surgery, it is deemed required. If a posterior laminectomy is done without cervical fusion, there is a small post-operative risk of developing instability that may lead to pain and deformity necessitating fusion at some point in the future.
